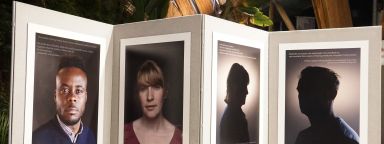
Space for Sharing Study
Researching online sharing by people in extreme circumstances.
People
Find contact details of those working on the project.
Funders and partners
Information on the funders and partners associated with the Space for Sharing study.
News and events
An archive of news and events for the project.





